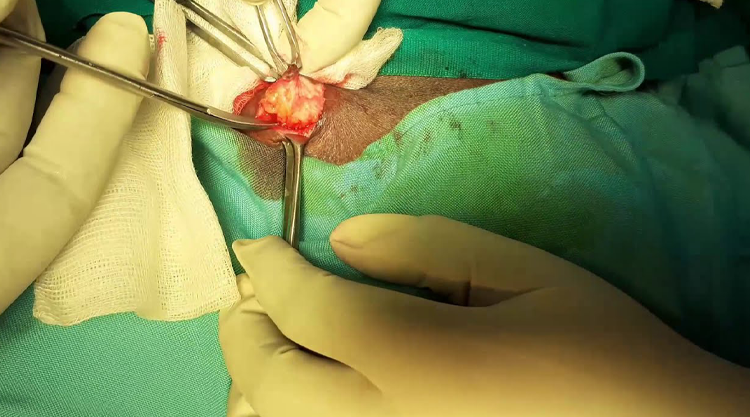
Perianal Abscess Drainage
An anorectal abscess is a collection of pus in the anal or rectal region. It may be caused by infection of an anal fissure, sexually transmitted infections or blocked anal glands.
The following anatomical types have been identified [1]:
- Perianal abscess: the most common (60%) - caused by direct extension of sepsis in the intersphincteric plane caudal to the perianal skin.
- Ischiorectal abscess: (20%) - results from extension of sepsis through the external sphincter into the ischiorectal space.
- Intersphincteric abscess: (5%) - depending on the effort made to find them, sepsis confined to the intersphincteric space.
- Supralevator abscess: (4%) - produces horseshoe abscess track.
- Postanal abscess: posteriorly based below the level of the ano-coccygeal ligament.
Who all can suffer with rectal abscess
- High-risk groups include those with diabetes, immunocompromised patients, people who engage in receptive anal sex and patients with inflammatory bowel disease.
- Deep rectal abscesses may be caused by intestinal disorders such as Crohn's disease or diverticulitis [2].
- Studies suggest that most patients are between the ages of 20 to 60 with a mean age of 40. The male-to-female ratio is 2:1 [3].
Presentation
- Symptoms include painful, hardened tissue in the perianal area, discharge of pus from the rectum, a lump or nodule, tenderness at the edge of the anus, fever, constipation or pain associated with bowel movements.
- The perianal pain is usually constant, throbbing and worse when sitting down.
- A rectal examination may confirm the presence of an anorectal abscess.
- Superficial perianal abscesses may occur in infants and toddlers. The abscess often appears as a swollen, red, tender lump at the edge of the anus. The infant may have discomfort but no other symptoms.
Fistula in ano [3]
- Fistulae occur in approximately 40% of patients with anorectal abscesses. Anorectal fistulae may also be associated with diverticular disease, inflammatory bowel disease, malignancy, tuberculosis and actinomycosis.
- One study found that 68% of recurrent abscesses were associated with a fistula.
- Goodsall's rule: an external opening situated behind the transverse anal line will open into the anal canal in the midline posteriorly. An anterior opening is usually associated with a radial tract. Goodsall's rule has been challenged as being inaccurate; cases have been reported where the external opening is off-midline [5].
- Fistulae may be classified as intersphincteric (25% in one study), trans-sphincteric (29.16%), suprasphincteric (8.33%), and extrasphincteric (12.5%). Extrasphincteric fistulae are usually not associated with intersphincteric sepsis [6].
Management
- Prompt surgical drainage.
- Medication for pain relief.
- Traditionally, antibiotics have not been considered necessary unless there was an underlying condition such as diabetes or immunosuppression. However, one study found that postoperative prophylactic antibiotic therapy including ciprofloxacin and metronidazole played an important role in preventing fistula-in-ano formation after incision and drainage of a simple perianal abscess [7].
- A Cochrane review found that fistula surgery with abscess drainage significantly reduced recurrence or persistence of abscess/fistula, or the need for repeat surgery, compared to abscess drainage alone [8].
- Low fistulae: lay open with either fistulotomy or fistulectomy[9].
- High fistulae: may require a defunctioning proximal colostomy; there is also a risk of postoperative faecal incontinence[10]. Faecal diversion, however, is not always necessary. One study described the treatment of high fistula by fistulectomy and reconstruction (primary suture repair) of anal sphincter without stool diversion [11].
- An advancement flap (a section of mucosa removed from the anal lining) may be used to close the defect. This technique has been found particularly helpful in Crohn's disease[12]. A biosynthetic anal fistula plug has been developed and the National Institute for Health and Care Excellence (NICE) recommends its use, providing standard consent and audit procedures are followed[13].
- Clinical trials assessing adipose stem cells, collagen, dermal matrix and numerous other techniques are ongoing [14, 15].
Complications
- Systemic infection.
- Fissure in ano occurs in up to 30% of patients (the risk is reduced by early surgical drainage).
- Recurrence.
- Scarring.
Prognosis
- The outcome is good if the abscess is treated promptly.
- Fistula in ano in children often resolves spontaneously and immediate surgical treatment should be withheld [16].
Anal fissures in children
The above measures apply to children who have a fissure as much as to adults. In children, the pain often makes them hold on to their stools. This may lead to a vicious circle, as then even larger and harder stools form. These then cause more pain when they are finally passed. Therefore, in addition to the above measures, a short course of laxatives may be prescribed for children with an anal fissure. The aim is to make sure their stools are soft and loose whilst the fissure heals.
What if the anal fissure does not heal with the above measures?
An anal tear (fissure) will usually heal within 1-2 weeks in most people. However, it can take longer to heal in others.
Glyceryl trinitrate ointment
If you apply glyceryl trinitrate (GTN) ointment to the anus, it relaxes the muscle around the anus (the anal sphincter). It also increases the blood supply to the damaged skin by dilating the blood vessels in that area. This may allow the fissure to heal better. It may also ease the pain. GTN ointment may help in some, but not all, cases. Research studies showed that, for people with a chronic anal fissure, about 6 in 10 fissures healed with GTN treatment. This compared to about 5 in 10 that healed with no treatment. So, the effect of GTN ointment is modest but may well be worth a try.
Other medicines
Some studies have shown that other medicines may also help to relax the anal sphincter muscle and increase the blood supply to the area, so helping healing of an anal fissure. For example, medicines called calcium-channel blockers, such as diltiazem. These medicines may sometimes be suggested for people unable to use GTN ointment.
An injection of botulinum toxin into the anal sphincter muscle has also been shown to relax the anal sphincter muscle and so help anal fissures to heal. This treatment may be suggested if other treatments have not been successful.
Surgery
An operation is an option if the fissure fails to heal or comes back. The usual operation is to make a small cut in the muscle around the anus (internal sphincterotomy). This permanently reduces the tone (pressure) around the anus and allows the fissure to heal. This is a minor operation which is usually done as day case surgery (you will not usually have to stay overnight in the hospital). The success rate with surgery is very high. At least 9 in 10 cases are cured.
Laser Ablation of the Fissure with Laser Anal Sphincterotomy is the latest advance in the surgery and it gives superior results in terms of minimum postoperative bleeding, negligible pain,faster recovery…and no cutting during the entire surgery.