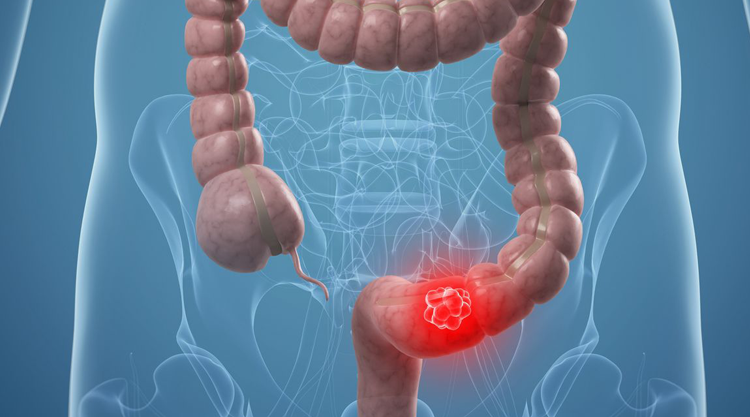
Colorectal Cancer
Most colorectal cancers are adenocarcinomas that evolve from polyps, which may be present for ten years or more before malignancy develops. Colorectal cancer is locally invasive but metastatic spread may be evident before local growth produces symptoms. The most common site for metastatic spread is the liver. Other sites (eg, the lungs, brain and bone) are unusual in the absence of liver metastases.
Risk factors
- Family history of colorectal neoplasia: carcinoma; adenoma under the age of 60 years[3] .
- Past history of colorectal neoplasm: carcinoma, adenoma.
- Inflammatory bowel disease: ulcerative colitis, Crohn's colitis.
- Polyposis syndromes: familial adenomatous polyposis (Gardner's syndrome), Turcot's syndrome, attenuated adenomatous polyposis coli, flat adenoma syndrome, hamartomatous polyposis syndromes (Peutz-Jeghers syndrome, juvenile polyposis syndrome, Cowden's syndrome).
- Hereditary non-polyposis colorectal cancer (HNPCC).
- Hormonal factors: nulliparity, late age at first pregnancy, early menopause.
- Diet: rich in meat and fat; poor in fibre, folate and calcium.
- Sedentary lifestyle, obesity, smoking, high alcohol intake.
- Diabetes mellitus.
- Previous irradiation, occupational hazards - eg, asbestos exposure.
- History of small bowel cancer, endometrial cancer, breast cancer or ovarian cancer.
Presentation
The presentation depends on the site of the cancer:
- Right colon cancers: weight loss, anaemia, occult bleeding, mass in right iliac fossa, disease more likely to be advanced at presentation.
- Left colon cancers: often colicky pain, rectal bleeding, bowel obstruction, tenesmus, mass in left iliac fossa, early change in bowel habit, less advanced disease at presentation.
- The most common presenting symptoms and signs of cancer or large polyps are rectal bleeding, persisting change in bowel habit and anaemia.
- All patients with symptoms suspicious of colorectal cancer must have a thorough abdominal examination and rectal examination.
- In some patients, symptoms do not become apparent until the cancer is far advanced.
- Jaundice and hepatomegaly indicate advanced disease with extensive liver metastases. Peritoneal metastases with ascites are often also present. 20-25% of patients have clinically detectable liver metastases at the time of the initial diagnosis and a further 40-50% of patients develop liver metastases within three years of primary surgery.
- Rarer clinical signs include: pneumaturia, gastrocolic fistula, ischiorectal or perineal abscesses, deep vein thrombosis.
Surgery remains the definitive treatment for apparently localised colorectal cancer. Both radiotherapy and chemotherapy can improve survival rates after potentially curative surgery.
If colonic stents are considered for patients presenting with acute large bowel obstruction, CT of the chest, abdomen and pelvis should be offered to confirm the diagnosis of mechanical obstruction, and to determine whether the patient has metastatic disease or colonic perforation[4] .
Surgery
May be performed either to attempt cure (removing the draining lymphatic field) or to relieve symptoms:
- Laparoscopic surgery has become the gold standard for surgical treatment. All the following described surgeries from the past, can now be performed with endoscopic instruments so that we have a better healing time, lesser pain and faster discharge.
- Right hemicolectomy: for tumours in the caecum, ascending and proximal transverse colon.
- Left hemicolectomy: if in the distal transverse colon or descending colon.
- Sigmoid colectomy: for tumours of the sigmoid colon.
- Anterior resection: if in the low sigmoid or high rectum. Anastomosis is achieved at the first operation.
- Abdomino-perineal (AP) resection: for tumours low in the rectum (less than approximately 8 cm from the anal canal). Permanent colostomy and removal of rectum and anus.
- However, a recent meta-analysis has shown no difference in oncological outcomes of laparoscopy for treating rectal cancer[11] .
- One of the most important advances for surgery of rectal cancer has been the concept of total mesorectal excision, which reduces local recurrences and peri-operative morbidity. The transanal route seems to be comparable to the laparoscopic route although further research is needed[12] .
- Pre-operative high-dose rate brachytherapy can be used in patients with cancer in the middle or lower third of the rectum to shrink the tumour. There is evidence for short-term safety and efficacy in reducing tumour bulk. However, there is no evidence for any additional benefit when used as a boost to external beam radiotherapy. Evidence on the clinical efficacy if used without external beam radiotherapy is inadequate in quantity[13] .
- All patients with resectable liver metastases should be considered for surgical resection.